Abstract
Introduction: Acute Myeloid Leukemia (AML) is an aggressive blood cell disorder that arises from clonal expansion of myeloid progenitors (blasts) in the bone marrow and peripheral blood as a result of gene mutation involved in hematopoiesis. In most cases, AML appears as de novo in a previously healthy person however, it can progress from myeloproliferative disorders (MPD) or myelodysplastic syndrome (MDS) as well. In this review, we highlight the baseline characteristics and outcomes in patients with AML and previous diagnoses of MDS or CML.
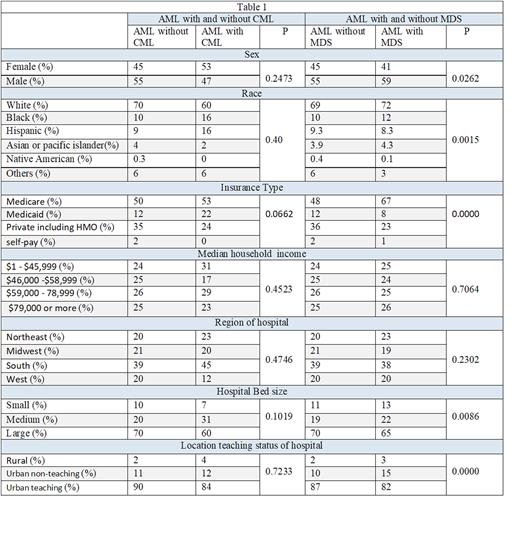
Methodology: Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS) was queried to identify AML admissions between 2016-2019 In Adult patients with a secondary diagnosis of MDS or Chronic Myeloid Leukemia (CML) using the International Classification of Disease 10th Revision (ICD-10) codes. We evaluated the baseline characteristics including Age, Sex, Race, Insurance type, Median household income, Region of hospital, Hospital Bed size, and Location/teaching status of hospital, in addition to mortality as the primary outcome and length of hospital stay (LOS) and total hospital charges (THC) as secondary outcomes.
Results: A total of 79579 patients with AML were hospitalized and among them, 4650 (6%) had a secondary diagnosis of MDS. The mean age of MDS group was higher (69.9 vs. 61.4) compared to those without MDS. In AML with the previous MDS, there was a significantly higher proportion of male sex, white race, Medicare insurance, rural and urban non-teaching hospitals with a higher proportion in small and medium-sized hospitals in comparison to those with AML without as reflected in Table (1). There was no difference in comorbidity burden, hospitalization region, and median household income. AML with a previous Diagnosis of MDS group had a non-significantly higher odds of mortality in comparison to patients without MDS (13% vs 11.8 %: AOR 0.91, p=0.41 CI 0.74-1.13). Females had non-significantly lower odds of mortality (0.89 with P=0.58). Among the secondary outcomes, the MDS group had lower mean LOS (15.3 vs 18,5) and lower THC ($214329. vs $254635) though statistical significance was not reached.
Also, among the AML group, 255 (0.3%) had a secondary diagnosis of CML. The mean age of patients with previous CML was higher (62.8 vs. 61.9) compared to patients without CML though not statistically significant. In AML with previous CML group, there was a higher proportion of female sex, black and Hispanic race, Medicaid insurance, lower household income, south hospitals region, medium sized hospitals in comparison to AML without previous CML though it was non-significant as reflected in Table (1). However, there was no difference in comorbidity burden. Those with a previous Diagnosis of CML had a higher odd of mortality in comparison to patients without CML though not statistically significant (17.5% vs 11.8 %: AOR 1.6, p=0.24 CI 0.72-3.54). black race had significantly higher odds of mortality (OR 9, P=0.018 CI 1.44-55.9) while Females had non-significantly higher mortality (3.85 with P=0.12). Among the secondary outcomes the CML group had a non-significantly lower mean LOS (15.9 vs 18) and lower THC ($ 231116 vs $254711).
Conclusion: In this analysis we found that sex, race, insurance type, median household income, and region of the hospital impact the risk of developing AML after MDS or CML. Prospective studies are required to look into the cause of these differences as it can be related to the socioeconomic disparities or specific gene mutations more prevalent in certain races of regions.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.